Although pulse oximeters were once predominantly used in medical settings, they are now commonly available to athletes. These small, yet powerful devices can give you a snapshot of your body’s ability to process oxygen, which is a key factor in performance if you live or train at altitude, or tend to overtrain. Here we’ll investigate how these devices work, and how you might use them to optimize your performance.
What Is a Pulse Oximeter?
A pulse oximeter is a device that measures blood oxygen levels (oxygen saturation or SpO2) by estimating the percentage of oxygen bound to hemoglobin in the blood. Pulse oximeters are small, portable, non-invasive and painless. They’re so convenient that they’re often used by pilots and people who work or train at high altitudes. Simply clip it to your finger, and it will give you an accurate data reading.
How Does a Pulse Ox Work?
When oxygen is inhaled into the lungs, it attaches to hemoglobin (a protein in red blood cells). The red blood cells then transport oxygen into the bloodstream, allowing it to be dispersed to tissue. Most of us need about 550 liters of oxygen per day to function, but that volume can double or triple during exercise. During low- to moderate-intensity exercise, your blood oxygen saturation will stay about the same as at rest. You may see blood oxygen levels drop during exercise at higher intensities (especially maximum aerobic intervals, about 3-6 minutes long) — or when you train at altitudes much higher than you are used to — but only slightly. As you train, your body will be able to utilize more oxygen more efficiently.
To find out how much oxygen is in your blood, a pulse oximeter emits light (typically red and infrared) through one side of your finger onto a photodetector on the other side. As it passes through your finger, the light hits your blood cells, and is absorbed differently by the hemoglobin without oxygen (deoxyhemoglobin) than by the hemoglobin with oxygen (oxyhemoglobin). The quality of the light that makes it to the photodetector can tell us how much oxygen is in your blood — normal ranges are typically from 94 percent to 100 percent.
Different oximeters are made for different purposes. Some are designed just for use in hospitals, but others can be more useful for athletic performance. The Masimo MightySat in particular offers four other metrics in addition to the standard blood oxygen saturation (SpO2). With heart rate (HR), respiration rate (RR), Perfusion Index (PI), and Pleth Variability Index (PVI), you can keep detailed tabs on your training progression, all of which can be synced to TrainingPeaks.
How to Use a Pulse Ox for Recovery
Using Peripheral Saturation of Blood Oxygen (SpO2) readings with your usual training metrics can, first and foremost, help you gauge whether you’re recovering properly.
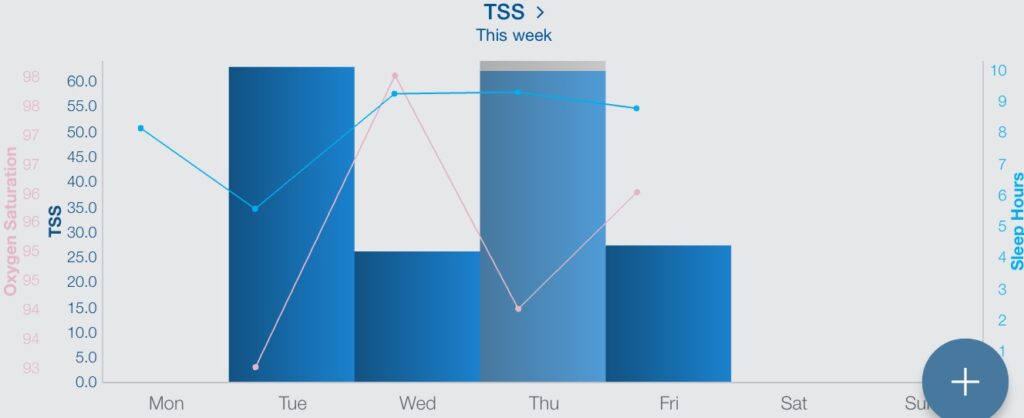
Take the athlete below, who woke up feeling “not right” after a hard training block. You can see the block in his Training Stress Score (TSS) for Tuesday. To make things worse, he was sleeping less than seven hours a night. Sure enough, he found that his morning SpO2 was low — just 93%.
This is a great case of an athlete who may feel well enough to go train, but his low sleep hours and low SpO2 corroborate his sense of “not feeling right.” Instead of continuing his training as planned, this athlete focused on recovery and sleep for the next two days (you’ll see he got nine hours of sleep for two consecutive nights). Subsequently, his SpO2 normalized and the following training days went very well.
Simply paying attention to the right numbers can result in a good training block and even help avoid an over-training scenario.
How to Use a Pulse Ox for Altitude Acclimatization
At altitude, where the air is thinner, it is more difficult for your body to get adequate oxygen to your muscles and tissues. For example, if you’re racing or training at 10,000 feet (3000 m), the amount of effective oxygen in the air is about 15% (compared to 21% at sea level). If you’re used to living at sea level, this change in oxygen availability will kick off a cascade of physiological adaptations, some of which are advantageous no matter where you’re racing.
To start, there will be an increase in your respiratory and heart rates; and the volume of blood ejected from the heart (stroke volume) will be reduced. Over your first 24-48 hours at altitude, blood plasma volume will also be reduced to improve the oxygen-carrying capacity of your blood by volume. These adaptations won’t necessarily feel good — in fact you’ll probably feel like you’re doing more work for less reward.
However, prolonged exposure to altitude will cause your body to increase production of red blood cells with larger hemoglobin, allowing for a partial or full restoration of the blood volume and arterial oxygen content. After four weeks or more, your maximal heart rate response will be lower, as will your peak cardiac output — your blood is carrying more oxygen, so your heart won’t need to pump as fast or hard.
Once fully acclimatized, your peak oxygen uptake will be the same as at sea level, but the saturation of arterial oxygen will be increased (i.e., you will have more complete oxygenation of the blood in the lungs). That means you’ll be able to race and train as normal at altitude, and will likely enjoy some extra aerobic endurance at sea level.
To understand what phase of acclimatization you’re in, and optimize your training around it, the Masimo MightySat can measure most of the adaptations mentioned above. Here’s what to look for in particular:
Blood Oxygen and Heart Rate
In the first couple of days at altitude, you want to see a lower Peripheral Saturation of Blood Oxygen (SpO2) and an elevated heart rate (HR) and respiratory rate (RR). This is your body attempting to balance out the lack of oxygen in the air by moving it faster through your body.
With prolonged stays at altitude, most people’s SpO2 will stay about the same or increase slightly; but your heart and respiratory rates should normalize, as well as your ability to perform exercise at altitude. A SpO2 of 88 to 92 percent will give you the most beneficial training adaptations without causing undue fatigue.
Dehydration
Another common problem at high altitudes is dehydration. Luckily the Mighty Sat has a parameter called the Pleth Variability Index (or PVI). It is a complicated measurement that ultimately shows your body’s hydration status, or ability to respond to additional fluids, way more accurately than the standard pee color test. For most people, if the PVI is 25 or above, it is safe to say that you should drink more. If it is below 20, you are probably fine. This is a great metric to use if you commonly find yourself dehydrated, or experience headaches at altitude.
Respiratory Rate Change
The Respiratory Rate (RR) function lets you gauge recovery after higher-intensity workouts. For example, if you know the time it takes your RR to come back to baseline after performing a five-minute interval at sea level, you will see that your RR takes longer to recover at altitude. As you acclimate, you should see the time for recovery drift back towards your baseline.
Note: If you find that you are not adapting at all after a couple of weeks, you may need to take a closer look at what is happening in your body. Several things could be going on, including inadequate iron intake, underlying sickness and overtraining (all good insights to have if you’re not seeing performance improvements!).
Whether you use a pulse oximeter for altitude training or to just monitor your recovery status, it is a simple and easy-to-use tool that can give you some really valuable insights.
Dr. Jonathan Edwards contributed to this article.










